Hot flash? More like HOT TOPIC!

Menopause has become the “hot” topic of conversation and although it is a natural stage of life that every woman will go through, each person can experience it in a different way. Of course, there are distinct and proven changes that occur in the body due to the physiological changes that come with menopause. But the severity, duration, and onset are different for everyone – and that’s okay! So let’s chat about what menopause is, what happens to our hormones, what body systems are impacted, and lastly what YOU can do before, during, and after to maintain a healthy and active lifestyle.
What is Menopause?
Menopause is defined by the stage in life in which a woman has their final menstrual period (FMP). The average age globally that women experience menopause is 51 years. “Early” menopause would be between the ages of 40-45 years. Anything prior to the age of 40 is considered premature ovarian insufficiency (this is rare, but possible).
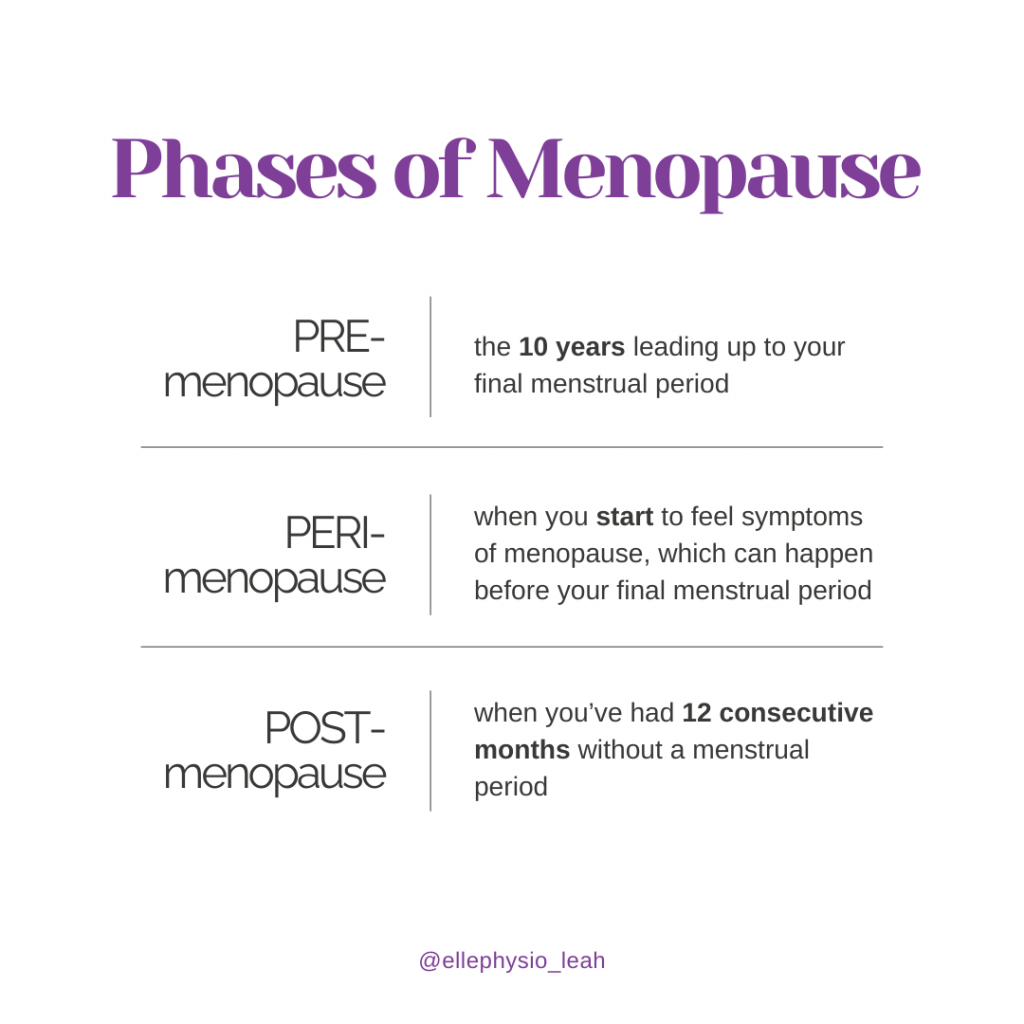
PRE-menopause is considered the time frame of the 10 years leading up to the FMP. Hormone changes begin, but are not noticeably symptomatic.
PERI-menopause is when you start to experience the symptoms of menopause, which can start well before your menstrual period ceases.
POST-menopause is when you have had 12 consecutive months without a period after your FMP.
What Happens to Our Hormones?
There are many hormones that support our bodies on a daily basis throughout our lifetime, but the ones we will focus on here are estrogen and progesterone. We know that menopause occurs due to a decline in ovarian function and decreased levels of estrogen and progesterone. This happens naturally with age, but can also be a streamlined transition due to hysterectomy/oophorectomy (removal of uterus and/or ovaries).
In PERI-menopause, we have HIGH estrogen and LOW progesterone. You can experience anovulatory cycles (periods without ovulation), anxiety, depression, insomnia, breast tenderness, heart palpitations, hot flashes/night sweats, headaches, and heavy, crampy, irregular periods.
In LATE peri-menopause and menopause, we have LOW estrogen and LOW progesterone. You can experience insomnia, musculoskeletal issues, arterial stiffening, genitourinary symptoms, and brain fog. Decreased estrogen also contributes to weight gain, belly fat, and central inflammation.
What Body Systems are Affected?
Sleep
Exhaustion and difficulty with sleep affects 84% of women going through menopause. Decreased sleep leads to increases in cortisol (the stress hormone). This affects our metabolism and hunger regulation, often leading to weight gain. Lack of sleep is directly linked to an increased risk of injury, slower recovery, and potential to develop chronic pain. When it comes to brain function, sleep allows the brain to learn new things every day while preserving and consolidating the old memories. Sleep is protective against dementia and other progressive cognitive conditions. In summary, this can manifest as muscle aches, decreased energy, brain fog, depression, anxiety, anger, increased stress, irritability and mood fluctuations, and decreased memory.
Hot Flashes and Night Sweats
These are called “vasomotor symptoms”, and they affect 70% of women going through menopause. The fluctuating levels of estrogen that occur in PERI-menopause is the main cause. We become more sensitive to changes in body temperature, requiring the body to respond and help regulate too often and too much, resulting in hot flashes. Once the estrogen levels steady again in menopause (despite being low), the hot flashes and night sweats tend to cease.
Genitourinary Changes
This includes changes in the vulvovaginal tissues, resulting in vaginal dryness and itching, pain with penetrative sex, decreased libido, impairment of arousal and orgasm, overactive bladder, incontinence, and increased risk of UTI and pelvic organ prolapse. Overall, the tissues related to all these structures need estrogen to function at their best. Without it, the tissues can become more rigid, dryer, thinner, and more susceptible to injury.
Weight Gain
Weight gain will often occur even without changing daily habits and lifestyle, due to the impact declining estrogen has on metabolism. Bloating and increases in belly fat are a product of low estrogen due to changes in insulin sensitivity, central inflammation, sleep issues, increased stress, digestive issues, and increased barriers to exercise (like incontinence!).
Heart Health
Decreases in estrogen leads to increases in LDL (bad) cholesterol and decreases in HDL (good) cholesterol. These changes in cholesterol lead to the development of atherosclerosis, or plaque in our arteries, placing women at higher risk of stress-related cardiac issues like heart attack, atrial fibrillation, stroke, and coronary heart disease.
Musculoskeletal Health
About 71% of women experience musculoskeletal pain in menopause. Joint pain is a result of sleep disruptions, loss of muscle strength, and increased inflammation, all because of (you guessed it) decreased estrogen levels. Tendons and ligaments are also impacted by estrogen levels – less estrogen results in stiffness and decreased tensile strength and ability to load the tissue, leading to increased risk of pain and injury. Cartilage volume also decreases which can contribute to osteoarthritic changes in the joints. Loss of muscle mass and strength naturally happens with age, and menopause contributes to this further.
Bone Health
Much like changes in muscle mass and strength, we naturally have a decline in bone mineral density with age, across men and women. However, women will experience further bone loss related to declining estrogen, placing them at higher risk for osteoporosis.
Brain Fog and Mental Health
Brain fog is reported by about 73% of women in menopause. This can be a result of the direct effects of declining estrogen levels, but also the impact of insomnia and sleep disturbances. The role that estrogen and progesterone have in mood and sleep place perimenopausal women at significantly higher risk of depressive symptoms and diagnoses. Furthermore, the drastic changes to genitourinary structures significantly impacts quality of life and self-esteem in women.
So What Can YOU Do?
First and foremost, speak to your primary healthcare provider
This is important to get the conversation started about what you’re experiencing physically and mentally, whether menopause hormone therapy (MHT) may be appropriate, and if any referrals to other healthcare providers may be warranted.
Menopause Hormone Therapy (MHT)
MHT can be systemic (via patch or gel), or local (applied vaginally only). It is not for everyone, but can provide significant treatment and mitigation of many symptoms of menopause. It is the gold standard for managing hot flashes, and significantly increases bone mineral density. It is a way to provide the body with estrogen that it is lacking, but it isn’t the ONLY way to treat! Talk to your doctor about your options.
Vaginal Moisturizer
There are hormonal (estrogen) and non-hormonal (hyaluronic acid) options. This is a local treatment to the vulvovaginal tissues to help with the hydration, elasticity, and pH levels of the tissues here. Vaginal moisturizer will help with dryness, irritation, stiffness of the tissues, but NOT urinary symptoms.
Pelvic Health Physiotherapy
Hi! Yeah, that’s us!! We are here to help you with any pelvic health concerns you may be experiencing through peri-menopause and beyond. We are experts in addressing overactive bladder, urinary incontinence, pelvic organ prolapse, and more. We help increase blood flow to the tissues, improve pelvic floor muscle strength, coordination, and relaxation, bladder training, and urge suppression. We may not be magicians but we sure do have many tricks up our sleeves!

Resistance Training
Heavy resistance training has been proven to be highly effective in mitigating menopausal symptoms. It creates an anti-inflammatory state, improves insulin sensitivity, improves mood, decreases weight gain and increases metabolism, improves brain function, decreases hot flashes, improves bone density, and improves heart health.
Sleep Hygiene
Some tips for improved sleep include avoiding blue light before bed, chamomile tea, bedtime stretching, restorative yoga, sniffing lavender oil, journaling to reduce worry and stress, creating a dark and cool sleep environment, and avoiding caffeine and alcohol later in the day. Create some sleep rituals that help signal your brain that it is time to rest and sleep!
Stress Management
The goal is not to remove all the stressors from your life (since that is virtually impossible), but give yourself tools to notice stress earlier, and manage it effectively. This may look like mindfulness and meditation, yoga, or breathwork.
Diet & Nutrition
Increased intake of protein helps with metabolism, hunger regulation, and building muscle mass. Plant-based proteins and high fibre are the most recommended.
Menopause can feel daunting, unpredictable and intense, but there are so many things YOU have control over that can help mitigate symptoms and make this natural transition in life much more manageable. And if you’re not sure where to start, talk to your primary healthcare provider to open the conversation. You might also consider working with a women’s health coach that is trained and educated on guiding women through this transition. It can be so hard to know where to start and what can help or hinder progress or symptoms in any one symptom category or more, a women’s health coach can go a long way to helping you navigate your options and empower you to make informed decisions on YOUR health (pssst….Karen San Andres is one!). You deserve to be seen and heard. You deserve to feel healthy and confident through menopause!
